Subdural Haematoma: what is it & why do I need to know about it?
Phil Wise explains via commonly held knowledge from public health resources such as the NHS and also his first hand account about what a Subdural Haematoma is & why you need to know about it.
Firstly – What is a Subdural Haematoma?
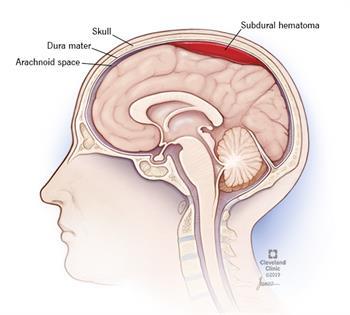
A subdural haematoma is a serious condition where blood collects between the skull and the surface of the brain. It’s usually caused by a head injury, and can occur even with relatively minor head injuries, depending upon the persons age. Commonly, this is know as a “bleed on the brain”.
A subdural haematoma occurs when a blood vessel in the space between the skull and the brain (the subdural space) is damaged.
Blood escapes from the blood vessel, leading to the formation of a blood clot (haematoma) that places pressure on the brain and damages it.
Head injuries that cause subdural haematomas are often severe, such as those from a car crash, fall or violent assault.
But minor bumps to the head can also lead to a subdural haematoma in some cases and the person may not even remember the bump or knock that caused it.
A minor head injury is more likely to lead to a subdural haematoma if you’re over 60, taking anticoagulant (“blood-thinning”) medicine or have a history of alcohol misuse.1
Are there different types of subdural haematomas?
Yes. Doctors sort subdural haematomas by how fast they develop, how much bleeding occurs, and how much damage the bleeding causes. The types of subdural haematoma are:
- Acute: This is the most dangerous type of subdural haematoma. Symptoms are severe and appear right after a head injury, often within minutes to hours. Pressure on the brain increases quickly as the blood pools. If not diagnosed and treated quickly, you could lose consciousness, become paralyzed or even die.
- Subacute: Symptoms usually appear hours to days or even weeks after the head injury. A subacute subdural haematoma can occur with a concussion.
- Chronic: This type of hematoma is more common in older people. Bleeding occurs slowly and symptoms may not appear for weeks or months. Even minor head injuries can cause chronic subdural haematomas. Due to the delay in developing symptoms, an older person may not even recall how their head injury happened. Also, the changes can be so subtle and occur so slowly that symptoms may not be noticed by the older person or their friends or family.
Are some people more likely to get a subdural haematoma?
Although anyone can get a subdural haematoma from an accidental head injury, certain groups of people are at higher risk. Subdural haematomas are more common in:

Older adults: As we age, our brains shrinks within our skull and the space between the skull and brain widens. This causes the tiny veins in the membranes between the skull and the brain to stretch. These thinned, stretched veins are more likely to tear in the event of even a minor head injury, such as a fall out of a chair.
Athletes who play contact sports: Football players and others who play high-impact sports and who might take a blow to the head have an increased risk of a haematoma.
Also, cycling is considered risky due to the high likelihood of falling, even with a helmet you can get a serious concussion (I did)

- People who take blood thinners: Blood thinners slow down the clotting process or prevent blood from clotting at all. If blood doesn’t clot, bleeding can be severe and long-lasting, even after a relatively minor injury.
- Hemophiliacs: Hemophilia is an inherited bleeding disorder that prevents blood from clotting. People with hemophilia have a higher risk of uncontrolled bleeding after an injury.
- Alcoholics and people who abuse alcohol: Drinking too much alcohol causes liver damage over time. Damaged livers can’t produce enough of the proteins that help the blood to clot, which increases the risk of uncontrolled bleeding.
- Babies: Babies don’t have strong neck muscles to protect themselves from trauma to the head. When someone abuses a baby by shaking him or her, the baby can develop a subdural haematoma. This type of injury is called shaken baby syndrome.2
What sort of symptoms would I have? – how would I know I had one?
Symptoms can be varied depending upon where exactly the haematoma is in the skull, but generally people will experience some common symptoms such as:
- a headache that doesn’t go away & keeps getting worse, (unlike tension headaches which come and go with changes in your stress levels)
- feeling and being sick
- confusion
- personality changes, such as being unusually aggressive or having rapid mood swings
- feeling drowsy
- loss of consciousness.1
There are additional symptoms2 including:
- Nausea and vomiting
- Slurred speech and changes in vision (and hearing/tinnitus, with photophobia in my own experience)
- Dizziness, loss of balance, difficulty walking
- Weakness on one side of the body (you can also get pins & needles & numbness in my own experience)
- Memory loss, disorientation, and personality changes, especially in older adults with chronic subdural hematoma
- Enlarged head in babies, whose soft skulls can enlarge as blood collects
As bleeding continues and the pressure in the brain increases, symptoms can get worse. Symptoms, at this point, include:
- Paralysis
- Seizures
- Breathing problems
- Loss of consciousness and coma
Why do you need to know about subdural haematoma?
Ok, so here is where the blog turns to being about my own personal account of subdural haematoma.
So what happened to me?
My past history includes a fall from a bike whilst wearing a helmet back in 2018, I had concussion but no other significant symptoms involving the nerves and was back to normal within 6 weeks. About 6 months after that I hit my head on a low oak beam in an old house and was concussed but back at work within about a month. Then, about a year later I hit my head again, but this time it was a relatively minor hit which ended up concussing me and causing me to be off work for a few weeks. So, you see I had a few head traumas already in a relatively short space of time.
Finally there was the creme de la creme of trauma to the head and that was a chance encounter with Maidstone’s finest of thugs whilst out walking one day and I was a victim of an unprovoked assault which resulted in me having broken facial bones and a concussion. I felt fine after a few weeks and was back at work like before.
Worrying symptoms
Then, at about 7 weeks after the assault, I noticed changes to my ability to control my left leg and arm/hand, followed by changes in my vision with an aversion to bright lights (photophobia) along with serious fatigue and poor coordination of my left hand, arm and leg (and later I had tinnitus develop too).
Surgery time
Due to the strains on the NHS, it took a whole a month before I was able to I have brain surgery, the first of which failed to provide resolution to the problem leading to further weakness, pins and needles (paraesthesia) in the left hand and also around my mouth, lips and tongue on the left side.

Subsequently, this required another surgery to relieve a further brain bleed which has so far proved successful in abating the headaches and photophobia, although all other symptoms remain at the moment, I’ve been assured by the consultant neurosurgeons at Kings College Hospital in London that all being well I should have a complete resolution to all my symptoms and be able to return to work within a few months. I of course remain hopeful, but time will tell.
UPDATE: I returned to work on 3/11/22 and am now happy to take your enquiries via telephone or book you in to see me in clinic.
WARNING: Don’t open this link if you’re at all squeamish – post operative scarring picture enclosed
Shown on the right are the Post Operative scars for ‘burr hole’ surgery.
Thankfully the removal of stitches has gone well and I seem to be recovering as well as can be expected from life saving surgery. I am of course ever grateful for the care and attention the NHS have shown me and particularly the surgeons and staff at Kings College London.

Takeaway points
The main point I wanted to make is this, be aware of these possibilities, as not all brain bleeds present as described in the medical texts and not everyone will have all of the symptoms I describe or what is described above in previous paragraphs. How it will affect you does depend on exactly where the haematoma is in the head, but generally speaking you will always have the symptoms listed above in the first paragraph under the heading of “What sort of symptoms would I have? – how would I know I had one?”.
Older?
You may be in the older age group and have some changes to your balance, a persistent headache, maybe some slight weakness in one or more of the limbs on one side of your body, or you might be a young person keen on sports who has had a relatively minor (so you think) injury to the head with no other symptoms except a persistent headache.
Active?
If you suspect that you have any changes at all in the way your body functions and you have had any kind of knock or trauma to the head or neck (such as a road traffic accident/whiplash) then please get yourself checked out fully by a medical professional, seeking second opinions if necessary and your symptoms are persistent beyond the first consultation.
Listen to your own body
I was initially told after the assault and subsequent A&E visit that there was no evidence of any subdural haematoma, it developed much later, about 6-8 weeks post trauma, which is the average time for a subdural haematoma to produce noticeable symptoms. Remember to seek a second opinion if in doubt and are concerned about ongoing symptoms as the sooner you have medical treatment, the sooner your brain can decompress and be further away from the danger of permanent damage.
As always if you need anything from us here at Baks then do please give us a call and we’ll do our very best to help you. You can call, text or email us.